Health in the periphery: the pharmacy of the future between technology and humanity
This is everyday life in many rural regions of Germany. It is quiet. Peaceful. But sometimes too quiet. Anyone who lives here knows the feeling: a cold is on the horizon, the fever is rising – but the nearest pharmacy is ten kilometers away. The bus doesn’t run again until the next day. The car is in the garage. And even if you could make it to the pharmacy: More and more often, there’s a “Closed” sign on the door.
In 2023, there were fewer than 18,000 pharmacies in Germany – the lowest number in over 40 years. On average, another one closes every week. This is particularly noticeable in sparsely populated areas. And while the infrastructure is thinning out, the population is ageing rapidly: by 2060, a third of Germans will be over 65 – with an increasing need for medication, diagnostics and personal advice.
But what will happen if these people soon no longer have anyone to care for them?
The vision for the year 2040 must address this question. It needs to think bigger – not just in terms of digital solutions, but in terms of a fundamental change in how medical care is organized. The pharmacy of the future could not only survive – it could become a central hub in the healthcare system.
One example: 3D printing of medicines. What sounds like science fiction has long been technologically feasible. The idea is simple: the patient receives a digital prescription from their GP or from a teleconsultation. This is transferred to a stationary medication printer at the local pharmacy or an automated pick-up point. A raw mixture is mixed with the appropriate active ingredient, melted and printed in exact doses – within a few minutes, individually tailored, without unnecessary waiting times. The technology is already particularly suitable for standardized medications such as paracetamol or ASA. In the future, however, it could enable patient-specific combinations of active ingredients, for example in cases of multimorbidity or chronic illnesses.
Telemedicine is a useful addition to this model. More than 1.4 million video consultations are already carried out in Germany every quarter. In many cases, a smartphone and an internet connection are all that is needed to speak to a doctor. Artificial intelligence is boosting this development: In breast cancer diagnostics, for example, AI has improved the hit rate by 11 percent. What is being tested in specialized clinics today could be part of everyday life in 2040 – as an assistance system for diagnosis, early detection and therapy planning.
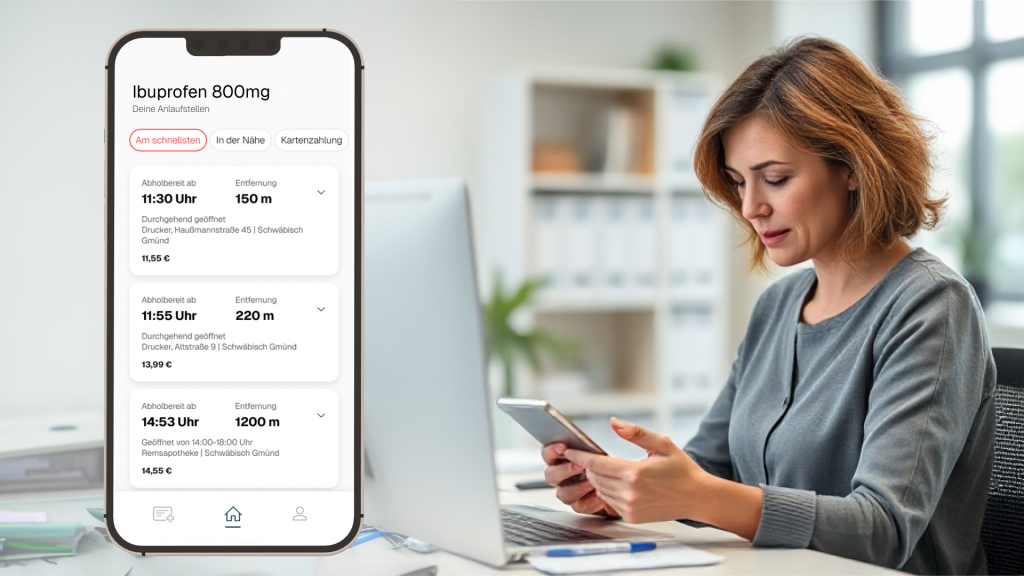
The role of platforms should not be underestimated. Services such as “IhreApotheken.de” or “MAYD” are already making it possible to order medicines from local pharmacies. The big tech companies have long been involved: Amazon bought PillPack and OneMedical, Alphabet took over Fitbit. The healthcare market has long since become a data market. This is where the opportunity lies – and at the same time the danger. Because when corporations take over the infrastructure, public players lose control over prices, access and data protection.
This is why a counter-model is needed: a platform organized by the state or a cooperative that connects pharmacies, doctors, health insurance companies and patients – openly, securely and independently. The aim is not to prevent technology, but to democratize it. Health must not be an exclusive product, but must be seen as a public good.
The platform of the future could achieve many things: diagnostic apps for different age groups and needs, accessible user interfaces for senior citizens, automatic reminders to take medication, direct prescription transmission, patient files, messages in plain language. Digital health applications (DiGAs) are already showing how great the need is – especially among women and in the 55 to 65 age group. The Corona-Warn-App has been downloaded over 48 million times. People are willing to use it if the offers are useful and trustworthy.
But despite all the digitalization, one thing must not be lost: the human aspect. Studies show that many people have a close emotional bond with their regular pharmacy – a bond that can hardly be found in any other sector. Pharmacies are easily accessible, often closer than a GP’s surgery. You don’t need an appointment, waiting times are short and personal contact is based on trust.
At a time when social media is increasingly replacing real interactions, many people have a growing need for real encounters. We are already experiencing a silent epidemic of loneliness – especially among older people. If pharmacies are degraded to purely digital interfaces, a place that does far more than dispense medication will be lost: It provides social care. It listens. It recognizes when a person is not feeling well – even between the lines.
The pharmacy of 2040 should therefore not only be smart, but also social. A place where technology helps, but does not replace. A place where the benefits of data and AI are used to create real time for real conversations. And a place where the healthcare system reinvents itself – not as a digital service, but as holistic care between humans, machines and compassion.
The future doesn’t have to be dystopian. But it will be if we don’t shape it.
Read more about the project medigo, which tackles this topic.